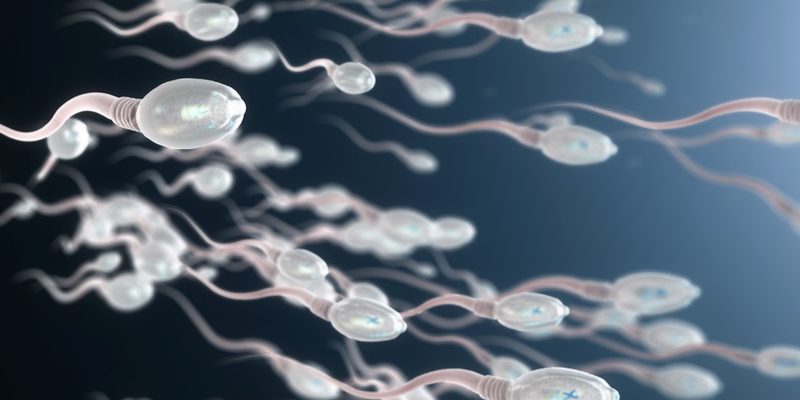
In humans sperm are produced in the testes and then migrate the epididymis; a small half-moon shaped organ attached to the testicles. The epididymis is a reservoir that allows the maturation of sperm during their journey to the vas deferens. The latter is attached to the prostate where sperm are mixed with prostatic secretions and those of the seminal vesicles thus producing seminal fluid. This seminal fluid eventually reaches the outside of the body through the urethra and the penis.
The initial assessment includes history and physical examination, two spermograms (1 month apart) and a hormonal assessment if the assessment or spermogram warrants it. Testicular ultrasound allows the evaluation of testicular volume and intra testicular pathologies. Thus the basic assessment makes it possible to discover certain causes of male infertility including varicoceles, obstructions of the genital tract, infections, immunological, hormonal or genetic abnormalities. Adjuvant examinations may be necessary including genetic evaluation; intra-rectal ultrasound and specialized sperm function tests (sperm DNA fragmentation). Grab more info about this and mainly the solutions there now.
History
In the questionnaire it is important to note the duration of infertility, the use of treatments and the possible presence of a concomitant factor in the spouse. One should also inquire about the frequency of intercourse, the use of lubricants and the possibility of sexual dysfunction.
The history of infant and pubertal development can reveal a delay in pubertal development or an absence of testicular descent (cryptorchidism) two conditions associated with male infertility. In addition, any history of trauma, genital infection (urethritis / prostatitis), systemic disease (diabetes, etc.) or pelvic or scrotal surgery is important.
Environmental toxins; alcohol, ionizing radiation, exposure to chemicals, especially smoking, can influence sperm production and quality. Also some drugs have a direct or indirect effect on hormonal balance or spermatogenesis.
Physical exam
The overall appearance and hairiness are important. The genital examination makes it possible to assess the scrotal content, ie the testicular volume, the absence of vas deferens or the presence of varicocele.
Varicoceles are the most common cause of male hypofertility. It involves dilation of the internal spermatic veins that drain the testicles. This condition is found in 40-50% of infertile men. (15% male population) Surgical correction or fluoroscopic embolization can be performed. An improvement in the quality / quantity of sperm in 50-75% of men is noted. Also the rate of spontaneous pregnancy is improved and possibly some couples can use less invasive techniques to arrive at conception (insemination instead of IVF / ICSI)
Spermogram (WHO / 2000)
Man produces ejaculate by masturbation or post-coitus with the use of a special condom. The sperm is examined immediately (<30-60 min post production). The main parameters evaluated are volume, quantity (conc / total quantity), motility (% motility) and morphology (% N forms). With the help of computers, we can qualify motility (fast: A / slow: B / stationary: C / immobile: D). It should be remembered that there is a daily variation in the quality of the sperm produced so it is therefore preferable to obtain two samples (delay 1 month, abstinence 2-3 days).
It is important to standardize the techniques of analysis and reporting of the spermogram. The parameters mentioned in the section are the last suggested by the WHO. In addition, a systematic assay of anti-sperm antibodies IgG, IgA is carried out.
Conclusion
An abnormal spermogram is usually associated with hypofertility more than infertility. Finally the evaluation of the functionality of the sperm requires certain tests specialized in investigation.











Comments